Understanding Frozen Shoulder: A Comprehensive Guide
Frozen shoulder, medically known as adhesive capsulitis, is a condition that leads to stiffness and pain in the shoulder joint. It develops gradually over time and can significantly limit the shoulder’s range of motion.
Causes and Risk Factors
The exact cause of frozen shoulder is often unclear, but it frequently follows a period of immobility or inactivity, such as after surgery or an injury. Additional risk factors include diabetes, thyroid disorders, and certain shoulder injuries or surgeries.
Stages of Frozen Shoulder
Frozen shoulder typically progresses through three stages:
1. Freezing Stage
This initial stage involves a gradual increase in pain and stiffness, restricting the shoulder’s range of motion and making daily activities challenging.
2. Frozen Stage:
During this stage, pain may decrease, but stiffness worsens, severely limiting shoulder movement.
3. Thawing Stage:
In this final stage, the shoulder slowly begins to improve, and the range of motion gradually returns. This stage can last from several months to a couple of years.
Treatment Options
Frozen shoulder typically progresses through three stages:
Treatment for frozen shoulder often includes a combination of pain management, physical therapy, and sometimes corticosteroid injections to reduce inflammation. In severe cases, surgery might be necessary to release the tight tissues around the shoulder joint.
Physical therapy is crucial for improving flexibility and strength in the shoulder. Here are some common physiotherapy approaches used for treating frozen shoulder:
1. Gentle Range of Motion Exercises:
Physiotherapists start with gentle exercises to gradually stretch the tight shoulder capsule. These may include pendulum exercises, wand exercises, or passive range of motion exercises.
2. Stretching Exercises:
Specific stretches target the muscles and tissues around the shoulder joint to improve flexibility and reduce stiffness.
3. Strengthening Exercises:
Strengthening exercises help stabilize the shoulder joint and enhance muscle strength, which aids in restoring function and preventing future injury.
4. Manual Therapy:
Techniques such as joint mobilizations and soft tissue massage can reduce pain, improve flexibility, and break up scar tissue or adhesions in the shoulder joint.
5. Modalities:
Physiotherapists may use heat, ice, ultrasound, or electrical stimulation to help reduce pain and inflammation.
6. Education and Home Exercise Program:
Physiotherapists provide education about the condition, posture, ergonomic principles, and home exercises to supplement in-clinic treatment. Consistent adherence to a home exercise program is vital for maximizing treatment outcomes.
7. Progressive Rehabilitation:
As the patient progresses, physiotherapy interventions are adjusted to match their improving condition, including advancing exercises and increasing resistance during strength training.
Get Started with These Exercises
Try these exercises to begin your journey to recovery, and book an appointment with one of our physiotherapists for expert advice and personalized help.
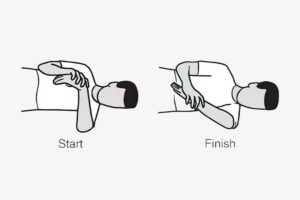
1) Pendular exercises

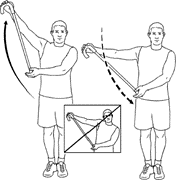
2) Active assisted Range of motion exercises


3) Capsular stretch: